REVIEW ARTICLE
ANXIETY AND DEPRESSION IN THE POSTPARTUM PERIOD: AN INTEGRATIVE LITERATURE REVIEW
ANSIEDAD Y DEPRESIÓN EN EL PUERPERIO: REVISIÓN INTEGRATIVA DE LA LITERATURA
ANSIEDADE E DEPRESSÃO NO PUERPÉRIO: REVISÃO INTEGRATIVA DA LITERATURA
https://doi.org/10.31011/reaid-2026-v.100-n.1-art.2621
1Kelvin Leandro Marques Monçalves
2Cláudia Zamberlan
3Josiane Lieberknecht Wathier
4Andressa da Silveira
5Júlia Oliveira Silveira
6Josi Barreto Nunes
7Larissa Bertoldo Vagner
8Keity Laís Siepmann Soccol
1Universidade Franciscana, Santa Maria, RS, Brazil. Orcid: https://orcid.org/0000-0001-5261-212X
2Universidade Franciscana, Santa Maria, RS, Brazil. Orcid: https://orcid.org/0000-0003-1898-328X
3Universidade Franciscana, Santa Maria, RS, Brazil. Orcid: https://orcid.org/0000-0002-5746-5349
4Universidade Federal de Santa Maria, Palmeira das Missões, RS, Brasil. Orcid: https://orcid.org/0000-0002-4182-4714
5Universidade Franciscana, Santa Maria, RS, Brazil. Orcid: https://orcid.org/0000-0001-5947-8875
6Universidade Franciscana, Santa Maria, RS, Brazil. Orcid: https://orcid.org/0000-0001-9364-841X
7Universidade Franciscana, Santa Maria, RS, Brazil. Orcid: https://orcid.org/0009-0000-3139-5031
8Universidade Franciscana, Santa Maria, RS, Brazil. Orcid: https://orcid.org/0000-0002-7071-3124
Corresponding Author
Keity Laís Siepmann Soccol
Rua Silva Jardim nº 1175, bairro Nossa Senhora do Rosário, Santa Maria-RS. Brazil - CEP: 97010-491 -phone: +55(55) 3025-1202 - E-mail: keitylais@hotmail.com
Submission: 06-08-2025
Approval: 12-11-2025
ABSTRACT
Objective: To identify evidence regarding anxiety and depression during the postpartum period and the impact of these conditions on women's lives. Method: An integrative literature review was conducted with the selection of 13 articles whose references met the research requirements within the time frame from 2018 to 2023. The scientific databases used were Latin American and Caribbean Health Sciences Literature, Nursing Database, National Library of Medicine, and SciVerse Scopus. Results: The analysis of the selected articles highlighted the relevance of comprehensive care for women's health from prenatal care through the postpartum period. Conclusion: This review emphasizes that pregnancy and the postpartum period are times of significant changes in a woman’s life and body. It underscores the importance of a comprehensive approach that considers both the physical and mental health of pregnant and postpartum women, including screening and treatment for mental disorders.
Keywords: Woman; Postpartum Period; Mental Health.
RESUMEN
Objetivo: Identificar la evidencia sobre la ansiedad y la depresión en el puerperio y la interferencia de estas condiciones en la vida de la mujer. Método: Revisión integrativa de la literatura con la selección de 13 artículos cuyas referencias cumplían con los requisitos de la investigación en el período comprendido entre 2018 y 2023. Las bases científicas utilizadas fueron Literatura Latinoamericana y del Caribe en Ciencias de la Salud, Base de Datos de Enfermería, National Library of Medicine y SciVerse Scopus. Resultados: El análisis de los artículos seleccionados evidenció la relevancia de la atención integral a la salud de la mujer desde el prenatal hasta el período puerperal. Conclusión: Esta revisión destaca que el embarazo y el puerperio son períodos de cambios significativos en la vida y en el cuerpo de la mujer. Se resalta la importancia de un abordaje integral que considere tanto la salud física como la salud mental de las gestantes y puérperas, incluyendo el cribado y los tratamientos para los trastornos mentales.
Palabras clave: Mujer; Período Posparto; Saludental.
RESUMO
Objetivo: identificar as evidências a respeito da ansiedade e depressão no puerpério e a interferência dessas condições na vida da mulher. Método: revisão integrativa da literatura com a seleção de 13 artigos cujas referências atendiam aos requisitos da pesquisa no recorte temporal de 2018 a 2023. As bases científicas utilizadas foram Literatura Latino-Americana e do Caribe em Ciências da Saúde, Bases de Dados de Enfermagem, National Library of Medicine e SciVerse Scopus. Resultados: A análise dos artigos selecionados, evidenciou a relevância da atenção integral à saúde da mulher desde o pré-natal até o período puerperal. Conclusão: esta revisão destaca que a gestação e o puerpério são períodos de mudanças significativas na vida e no corpo da mulher. Destaca-se a importância de uma abordagem integral que considere tanto a saúde física quanto a saúde mental das gestantes e puérperas, incluindo triagem e tratamentos para transtornos mentais.
Palavras-chave: Mulher; Período pós-parto; Saúde Mental.
INTRODUCTION
Puerperium is marked by the restoration of the organism to preconceptional conditions, during which biological, psychological and emotional changes occur. These changes increase the potential for complications that, when not recognized and treated, can result in maternal morbidity and mortality due to causes that could be prevented (1).
Stress is a set of reactions so that the body sends out a warning signal to what has been manifested. When the body feels threatened, the body starts a process with physical and emotional changes, causing the body to start demanding more and more energy. As consequences of chronic stress, the emergence of disorders such as anxiety and depression are presented in the individual. Important changes in daily and life, such as the postpartum period, can generate often unsympathetic responses to stress (2).
The female gender is recognized as one of the specific variables in the sequence of events that lead to depression, and women are more likely than men to experience depressive disorder at some point in their lives (3-4), including in the postpartum period.
Considering that the rate of postpartum depression (PPD) in Brazil is 26%, being higher than the average established by the World Health Organization (WHO) for low-income countries (Maciel et al., 2019), it is crucial that health professionals start monitoring, if possible, in the immediate puerperium (1st to 10th day), to detect signs and symptoms of psychological changes during the consultation or home visit, take appropriate measures and refer cases in a timely manner (5).
In addition to the typical symptoms of depression in the general population, such as depressed mood, loss of interest, feelings of low self-esteem and decreased concentration, the postpartum period is marked by hormonal changes and alterations in family dynamics and the mother’s relationship with the baby (6). PPD is also associated with sexual difficulties, such as decreased libido, which can affect a woman’s affective relationships with her partner (7).
Studies have observed elements that predispose cases of PPD and postpartum anxiety, which include: family or personal history of depression, lack of social and economic support, interference in the conjugal relationship, low self-esteem, obstetric complications, conflicts in family relationships and unwanted pregnancy (8-9). Unlike PPD, puerperal anxiety (PA) is characterized by restlessness, irritability, fatigue, difficulty concentrating and lack of sleep. Given the changes that occurred from conception to puerperium, the woman presents doubts, fears, insecurities and fear about her ability to care for the newborn (RN) in a correct way (10).
The presence of an adequate social-family support, especially on the part of companion, plays a crucial role in mitigating the effects of anxious symptoms. When this support is insufficient, the relationship between mother and baby can become challenging, manifesting both in the form of deficiency and excess, which results in symptoms that disturb the family dynamics (11).
To prevent the consequences of PPD and PA, both should be observed and treated early. In this sense, it aimed to identify the evidence regarding anxiety and depression in the puerperium and the interference of these conditions in the life of women.
METHODS
This is an integrative review, a research method that summarizes literature research results through a systematic analysis process. Articles published in full were included, freely available and indexed in the databases in Portuguese, English or Spanish, with publication date in the last five years, because they represent more current productions related to the theme under study. Duplicate publications, experience reports, editorials, dissertations, theses, reviews and incomplete articles were excluded.
The following steps were used for the review: 1) elaboration of the research question ("What are the available scientific evidence on the occurrence of anxiety and depression in the postpartum period and how do these conditions interfere with the life and well-being of women?" ); 2) searches the literature of primary studies based on inclusion and exclusion criteria; 3) organization of pre-selected studies (data extraction from primary studies); 4) critical analysis of selected primary studies; 5) analysis and synthesis of evaluated results; 6) presentation of the integrative review (12).
The searches occurred between August and September 2023, the databases where the searches took place were Latin American and Caribbean Literature in Health Sciences (LILACS), Online System for Search and Analysis of Medical Literature (MEDLINE), Nursing Database (BDENF) and SciVerce Scopus. Using the descriptors indexed in the Health Sciences Descriptors (DeCS), the combinations used are described in Chart 1, below:
Chart 1 – Search strategy for the review study.
|
Descriptors (DeCS/MeSH) |
Related Subjects |
Boolean Combination Used |
|
Saúde da mulher (Women’s Health) |
Specific health conditions of the female sex; comprehensive care for women; physical, mental and social well-being. |
Saúde da mulher AND depressão AND ansiedade AND período pós-parto |
|
Depressão (Depression) |
Depressive disorders; affective symptoms; postpartum depression; psychosocial impact on maternal health. |
Saúde da mulher AND depressão AND ansiedade AND período pós-parto |
|
Ansiedade (Anxiety) |
Anxiety symptoms; emotional disturbances; psychological stress; anxiety disorders in the pregnancy-puerperium cycle. |
Saúde da mulher AND depressão AND ansiedade AND período pós-parto |
|
Período pós-parto (Postpartum Period) |
Postpartum period; maternal adaptation; hormonal and emotional changes; care for the mother and newborn. |
Saúde da mulher AND depressão AND ansiedade AND período pós-parto |
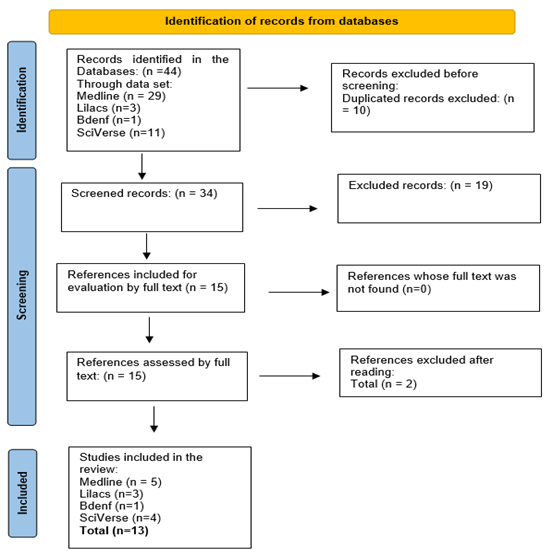
The articles found in the four databases were obtained from searches conducted in the Virtual Health Library (VHL) for MEDLINE, LILACS, BDENF, and on the SciVerse Scopus platform. We used the mentioned descriptors and listed the main subjects, such as: Anxiety; Postpartum depression; Depression; Postpartum period; Anxiety disorders; Women’s health; Mental health. A total of 44 articles were found, being: MEDLINE: 29 articles; LILACS: 3 articles and BDENF: 1 article; SciVerse Scopus: 11.
RESULTS
The articles selected to contain this study were reviewed by two independent reviewers according to the inclusion and exclusion criteria. The search and selection of articles are described in Figure 1 (Flowchart related to the selection process of articles according to PRISMA/2020) (13).
Figure 1 - Flowchart related to the selection process of articles according to PRISMA/2020
The main results of the analyzed articles will be presented below, having been grouped in Table 1 for better visualization and understanding. For the critical evaluation, a complete reading of the studies was carried out in order to identify relevant aspects that were repeated or stood out. The articles found were characterized according to the following data: identification code; authors/year; objective and results.
Table 1 - Corpus of analysis of the articles. Composed of identification number, authors, year, and main results.
|
PLACE |
RESULTS |
|
|
Suryawanshi, Pajai, 2022. (14) |
United States of America |
Postpartum depression (PPD) is a common and serious condition affecting mothers after childbirth, with negative impacts on child development and maternal mental health. It is associated with psychological factors and the use of medications such as methyldopa. Diagnosis can be made with the EPDS and clinical assessments. Treatments include SSRIs, tricyclic antidepressants, and psychological therapies, with brexanolone being a recent highlight. Early diagnosis and appropriate care are essential for prevention and effective management. |
|
Gete, et al. 2021(15) |
Israel |
The study revealed that immigrant mothers in Israel have a higher prevalence of postpartum mental disorders, such as depression, anxiety, and stress, compared to native mothers. Psychological scales applied, such as the Edinburgh Postnatal Depression Scale (EPDS) and the Hamilton Anxiety Scale (HAM-A), indicated significantly higher scores among immigrant mothers. Factors such as language barriers, social isolation, and challenges of cultural adaptation were identified as contributing factors to these symptoms. The study emphasizes the need for specific psychological screening and adequate support for immigrant mothers to improve the early identification and management of postpartum mental disorders. |
|
Lee-Carbon et al. 2022(16) |
England |
Two hundred women met the diagnostic criteria for a mental disorder. 34% had at least one contact with mental health services. Moderate depression, severe depression, prior psychiatric hospitalization, symptoms of anxiety, and perception of low levels of social support were associated with a higher likelihood of contact with mental health services in univariate analyses. However, moderate support and severe depression remained significant in multivariate regression analyses. |
|
Nanjundaswamy, et al. 2020. (17) |
India |
Of the 118 obstetricians who responded to an online survey, most were contacted due to concerns about hospital visits (60.17%), baby safety (52.14%), anxieties related to media news (40.68%), and contracting the infection (39.83%). Obstetricians felt the need for resources such as videos, relaxation techniques, and counseling skills to deal with COVID-related anxiety among perinatal women. |
|
Osborne, Kimmel, Surkan, 2021(18) |
United States of America |
Increased depressive symptoms during the COVID-19 pandemic, with a 40% increase in depression and a 60% increase in anxiety. Disproportionate impact on racial communities, where mortality rates and higher risk of infection are greater among Black women. Additional challenges in disadvantaged communities, those already facing socioeconomic problems, food insecurity, housing, violence, etc., but also an opportunity for the expansion of telemedicine, as well as a need for further research to understand the impact of stress. |
|
Overbeck, et al. 2022(19) |
Denmark |
There were no differences in reported levels of depressive symptoms across the six-month time period examined during the pandemic. Specifically, symptoms remained unchanged after the first lockdown. No significant changes were observed in anxiety symptoms in relation to increased infection pressure or lockdowns, but a slight increase was observed during the second lockdown in women 8 weeks postpartum. |
|
Gopalan, et al. 2022(20) |
United States of America |
Postpartum depression (PPD) is strongly associated with risk factors such as a history of mental disorders, lack of social support, socioeconomic stress, and adverse experiences during pregnancy. The COVID-19 pandemic exacerbated these risks, especially among Black women, contributing to increased maternal mortality rates. In response, the authors suggest implementing integrated care models and intergenerational approaches as effective strategies to improve screening, prevention, and access to PPD treatment, promoting positive changes in maternal health at the population level. |
|
Segamarchi, et al. 2021(21) |
Brazil |
Clinically significant levels of depression were found in 47.7% of participants, clinically significant levels of generalized anxiety in 41.8% of cases, and comorbid symptoms in 33.1% of the sample. |
|
Çankaya, Simsek, 2021(22) |
Turkey |
Women who participated in prenatal education sessions showed significant reductions in levels of fear of childbirth, depression, anxiety, and stress symptoms, as well as an increase in childbirth-related self-efficacy, compared to the control group (p<0.05). In the postpartum period, these positive effects were even more pronounced (p<0.001). Furthermore, the group that received prenatal education had a significantly higher rate of vaginal deliveries compared to the control group (p=0.043). |
|
Mateus, et al. 2022(23) |
Brazil |
The prevalence of clinically significant depression, anxiety, and comorbid symptoms was 26.7% and 15.2% in pregnant women and 32.7%, 26.6%, and 20.3% in postpartum women. Significant differences between countries were found in all mental health indicators in both perinatal periods. Higher levels of symptoms were observed during the pandemic, especially among postpartum women. |
|
Mesquita, et al. 2023(24) |
England |
The participants were 7,645 pregnant women or postpartum mothers with babies up to 6 months old who completed the Edinburgh Postnatal Depression Scale (EPDS) or the Generalized Anxiety Disorder Assessment. |
|
Muller, et al. 2021(25) |
Brazil |
Most postpartum women (81.2%) did not present with depression or had mild depression, 14.4% had mild to moderate depression, and 4.4% had moderate to severe depression. Regarding anxiety, 68.4% presented with minimal anxiety, 21.6% with mild anxiety, 7.6% with moderate anxiety, and 2.4% with severe anxiety. As for factors associated with postpartum depression, no sociodemographic or childbirth-related variable showed an association. Regarding anxiety, yellow/indigenous skin color, lack of paternal support, and pregnancy interruption were associated with more advanced anxiety levels. |
|
Quevedo, et al. 2021(26) |
Brazil |
The first assessment took place during the prenatal period, and the second occurred between 30 and 60 days postpartum. The incidence of postpartum suicide risk was higher in mothers with postpartum depression, and higher in those with mixed episodes, than in those who did not suffer from any mood disorder. |
Of the included studies, eight were published in international journals and five in national journals. With respect to the year of publication, the included studies were published between 2020 and 2023. As for the research site, it is observed in Table 1 that the studies have global scope, being four from Brazil, two from England, one from India, one from Turkey, one from Denmark, one from Israel and three from the United States of America. Concerning the languages, eight of the publications used the English language and four, the Portuguese language.
Regarding the contents, the studies focused predominantly on the symptoms of anxiety and depression during the perinatal period, the prevalence and diagnosis of mental disorders, and on the impact of the COVID-19 pandemic on perinatal mental health.
DISCUSSION
The high prevalence of postpartum depression and the lack of mental health services make effective intervention in the puerperal period urgent (27). With a high rate involving mental health cases in puerperal women and based on the principle of integrality, which refers to looking at the subject as a whole, it is important to recognize that Primary Health Care (PHC) has key responsibilities in the mental health care of women during pregnancy and puerperium (26).
When the prior mental condition of a woman with predisposition to mental disorders is not assessed and proper care is not provided, in many cases there is a risk of suicide. The psychiatric problems most consistently linked to suicide risk are mood and anxiety disorders. Mothers with previous and postpartum anxiety disorders are seven times more likely to be at risk of suicide (28).
Puerperium, in addition to the significant changes it brings to women, drastically affects the life of the couple, bringing moments of insecurity, instability and difficulties that will affect over the period. It is essential that the partner be included in this new routine, becoming available to care for the NB and domestic tasks, in order to avoid the emotional and physical wear of the woman and, consequently, develop affection and bond formation with the baby (22).
While most women will not have depressive or anxiety symptoms during the perinatal period, some will experience these symptoms with varying degrees of severity, indicating a need for continuous screening over time. Health professionals should make use of devices and tools for this identification, allowing them to diagnose women with a higher risk of developing PPD and postpartum anxiety, which may alter the course of maternal mental health symptoms (14-16).
A study shows that just over one-third of women who met the diagnostic criteria for a mental disorder in the first trimester of pregnancy did not seek professional help in the following year. This highlights the importance of universal mental health screening during the perinatal period to identify those at risk for mental disorders and establish clear pathways for referral to services when needed. It also highlights that women with moderate to severe depressive symptoms were more likely to seek mental health services during pregnancy and up to three months after delivery (29).
With the high prevalence of anxious and depressive symptoms in women in the puerperal period, it becomes essential to qualify health professionals to address the issue during the consultation. Considering that the professional nurse is who coordinates educational actions in the Family Health Strategy, it is relevant to understand the factors that can lead to a PPD, often overlooked by professionals. Improving care based on current studies can encourage, raise awareness and train professionals and students about the importance of quality care that, when used in a timely manner, provides early treatment and recovery from puerperium (9).
There are tools for the early identification of perinatal anxiety or PPD during prenatal and puerperal consultation, starting with therapeutic listening assisted by a quality consultation where there is information that this woman understands and makes use of them. Existing scales can also be used, such as the Edinburgh scale (22). The Edinburgh Postpartum Depression Scale (EPDS) is one of the useful tools for screening perinatal disorders, and now also recognized as a screening tool for anxiety. It is possible to perform a comorbid or primary perinatal screening. Pregnant and postpartum patients should be screened at the first consultation and postpartum delivery with EPDS, whereas patients with high-risk pregnancies or premature births should be screened more frequently (30).
There are multiple factors for an increase in cases of PPD, including lower maternal schooling, the presence of a partner, gestational planning and skin color (31-32). With regard to demographic and health conditions, there was no association with PPD in relation to anxiety; however, yellow/indigenous color and black women, lack of paternal support and having interrupted pregnancy were associated with more advanced anxiety conditions (18).
The disadvantages among black and brown women went beyond economic factors, evidencing the lower utilization of health services and thus increasing the likelihood of developing the disease. In the state of the Amazon and the Northeast region, 28.4% of cases were found in black women. In Salvador and the study that analyzed Recife and Campinas, the rates were even higher, 46.7% and 65.1%, respectively (33).
In a cross-sectional study carried out in a large city of the interior of São Paulo, 186 women with 60 days postpartum were analyzed. Among them, 138 belonging to the black race, ie black and brown. The study identified that 24.2% of participants presented indicative of depressive disorder. Among the risk factors for PPD, child abuse, unemployment, low empowerment, lack of social support, history of fetal losses and grief, marital instability, add to such factors issues of race, considering structural racism, financial difficulties, preference for the sex of the child, thought about interrupting pregnancy and non-acceptance of pregnancy increase during the third gestational period (1,23).
In addition, this review presented as results an expressive amount of studies on postpartum anxiety and depression related to the COVID-19 pandemic. There was a high global prevalence of clinically significant symptoms of depression, anxiety and refractory depression in women in the puerperal period (23, 34). The worsening of symptoms was related to social isolation, concerns and fears about the NB, economic uncertainties and lack of family support (34).
Quality care during pregnancy and puerperium is associated with better perinatal outcomes. The difficulty of access to health services, distance from their support networks and the overload of news with the increasing number of deaths due to coronavirus significantly increased anxiety and depressive symptoms in postpartum women, compared to pre-pandemic numbers (29,35).
Containment health measures were associated with better prenatal mental health outcomes in the initial period of the pandemic; while a nonlinear effect was observed in the puerperal period. Country-related and individual factors explain part of the variability in this association, with women from more disadvantaged countries at greater risk of adverse mental health outcomes (17). Anxiety related to COVID-19 during pregnancy needs to be addressed, as anxiety can adversely influence pregnancy and outcome (19). The early identification of mental health problems in perinatal women is therefore essential for obstetrics providers to collaborate with mental health specialists to offer appropriate interventions (36-37).
In Denmark, the study failed to demonstrate a clear mood change among pregnant women during different stages of the pandemic. However, since pregnancy and childbirth are vulnerable periods of life, caregivers should pay attention to the mental health of new mothers, which suggests that the possible consequences of the pandemic on mental health will be long-term and must be monitored (19).
The association of the integral look, technical-scientific knowledge by the nurse during pregnancy, together with the skill of qualified listening and empathy, ambience so that this woman feels welcomed and respected, strengthening ties and hearing their doubts, creates a solid foundation for pre- and post-natal care (36). However, proposing public policies that can prevent PPD, using tools that enable an early diagnosis and providing professionals with knowledge are essential for a good prognosis (38).
It is further emphasized the offer of a qualified health care, where you can understand the pregnant/ puerperal in its entirety, aiming at their health as a whole, not only physical, but also her mental health by providing sufficient subsidies and knowledge so that she can recognize the signs and symptoms and also know who to ask for support (36-38).
The above findings show the importance of psychological prenatal care linked to physical prenatal care, playing a crucial role in caring for the emotional well-being of pregnant women. This allows a comprehensive approach to the health care of women during this phase of their lives and will also help signs of anxiety and depression to be identified and treated correctly during pre-partum, childbirth and puerperium.
FINAL THOUGHTS
The study demonstrated that the symptoms of anxiety and depression during the perinatal period of higher reported prevalence were associated with: prenatal anxiety, pre-natal depressive symptoms and in early puerperium and lower age of mothers. The prevalence and diagnosis of mental disorders arise when: there is anxiety about pregnancy and childbirth, being a non-Caucasian woman, not having a stable relationship, lack of parental support and being young. The impact of the COVID-19 pandemic on perinatal mental health evidenced an increase in cases of anxiety during the pandemic and the need for mental assessment during prenatal care.
Although relevant, the resources and attention in the perinatal and puerperal area are directed to the newborn, often neglecting the postpartum mental state. The physical and mental changes that occurred in this period are interconnected, and mental health problems can negatively affect the interpersonal relationship of the mother-baby binomial.
It is also important and necessary to address issues of mental health during pregnancy that extend into the postpartum period, offering support to women and providing quality care and information. In short, the importance of care for the mental health of puerperal women is highlighted, emphasizing the need for an integral approach that covers both physical and mental health, with screening and appropriate treatments to prevent and diagnose early mental disorders.
REFERENCES
1. Lima RVA, Melo LCO, Barbosa NG, Arciprete APR, Monteiro JCS. Depressive disorder among postpartum women: an analysis according to self-reported race/color. Acta Paul Enferm 2023;36:eAPE03451. DOI: 10.37689/acta-ape/2023AO034511
2. Souza NKP, Magalhães EQ, Rodrigues Junior OM. The prevalence of postpartum depression and its consequences in women in Brazil. RSD [Internet]. 2021;10(15):e597101523272. DOI: https://doi.org/10.33448/rsd-v10i15.23272
3. Fernandes TB, Carmo LR, Araujo M, Moreira SA, Macêdo JP. Transtornos do Humor: Depressão e Transtorno Bipolar: Uma análise dos sintomas, diagnóstico e opções de tratamento para transtornos de humor, como a depressão e o transtorno bipolar. Braz. J. Implantol. Health Sci [Internet]. 3º de outubro de 2023;5(5):173-87. DOI: https://doi.org/10.36557/2674-8169.2023v5n5p173-187
4. Gutiérrez-Rojas L, Porras-Segovia AA, Dunne H, Andrade-González N, Cervilla JA. Prevalência e correlatos do transtorno depressivo maior: uma revisão sistemática. Debates em Psiquiatria [Internet]. 2022];12:1-44. DOI: https://doi.org/10.25118/2763-9037.2022.v12.464
5. Oliveira DBB, Santos AC. Saúde mental das gestantes: a importância dos cuidados de enfermagem. Rev JGR Estudos Acadêmicos. 2022;5(11):97-108. DOI: https://doi.org/10.5281/zenodo.7116674
6. Campos RB, Pinto AAVC, Cunha GS, Bispo AN. Análise sobre a depressão pós-parto e fatores associados à sua prevalência. Braz. J. Hea. Rev [Internet]. 2024;7(10):e75089. DOI: https://doi.org/10.34119/bjhrv7n10-101
7. Johannes CB, Clayton AH, Odom DM, et al. Distressing sexual problems in United States women revisited: prevalence after accounting for depression. J Clin Psychiatry. 2009;70(12):1698-1706. DOI: https://doi.org/10.4088/JCP.09m05390gry
8. Martins FM, Araujo LMB, Amâncio NFG, Silva JL. Os fatores desencadeantes e sintomas associados à depressão pós-parto. Braz. J. Implantol. Health Sci [Internet]. 2024;6(2):222-4. DOI: https://doi.org/10.36557/2674-8169.2024v6n2p222-242
9. Nascimento FCA, Carmo TN, Costa RSL. Fatores associados à depressão pós-parto em mulheres adolescentes. Dec.Foco [Internet]. 202;7(2):75-86. Available from: https://revistas.uninorteac.edu.br/index.php/DeCienciaemFoco0/article/view/201
10. Delfino JA, Melo AKP, Bernardes IAS, Diniz, ALX, Almeida CS, Souza DAS. Ações educativas para a gestante no pré-natal acerca dos cuidados com recém-nascido. Saúde Coletiva. 2021;11(63):5362-375. DOI: https://doi.org/10.36489/saudecoletiva.2021v11i63p5362-5375
11. Pinto CSP, Almeida CMT, Castro JF. Factors associated with levels of anxiety in postpartum women hospitalized in an obstetrics service. Mundo Saude [Internet]. 2023;47:e15162023. DOI: https://doi.org/10.15343/0104-7809.202347e15162023P
12. Souza MT, Silva MD, Carvalho R. Integrative review: whats it is? How do it?. Einstein. 2010;8:102-106. Available from: https://www.scielo.br/j/eins/a/ZQTBkVJZqcWrTT34cXLjtBx/?format=pdf&lang=pt
13. Page MJ, McKenzie J, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372(71). DOI: https://doi.org/10.1136/bmj.n71
14. Suryawanshi O, Pajai S. A comprehensive review on postpartum depression. Cureus. 2022;14(12):e32745. DOI: https://doi.org/10.7759/cureus.32745
15. Gete SL, Gete M, Levy R, Kurzweil Y, Margalit RC. Comparing the different manifestations of postpartum mental disorders by origin, among immigrants and native-borns in Israel according to different mental scales. Int. J. Environ. Res. Public Health. 2021;18(21):11513. DOI: https://doi.org/10.3390/ijerph182111513
16. Lee-Carbon L, Nath S, Trevillion K. et al. Mental health service use among pregnant and early postpartum women. Soc Psychiatry Psychiatr Epidemiol. 2022;57:2229-40. DOI: https://doi.org/10.1007/s00127-022-02331-w
17. Nanjundaswamy MH, Shiva L, Desai G. et al. COVID-19-related anxiety and concerns expressed by pregnant and postpartum women a survey among obstetricians. Arch Womens Ment Health. 2020;23:787-790. DOI: https://doi.org/10.1007/s00737-020-01060-w
18. Osborne LM, Kimmel MC, Surkan PJ. The Crisis of Perinatal Mental Health in the Age of Covid-19. Matern Child Health J. 2021;25:349-352. DOI: https://doi.org/10.1007/s10995-020-03114-y
19. Overbeck G, Rasmussen IS, Siersma V. et al. Mental well-being during stages of COVID-19 lockdown among pregnant women and new mothers. BMC Pregnancy Childbirth. 2022;22(92). DOI: https://doi.org/10.1186/s12884-021-04374-4
20. Gopalan P, Spada ML, Shenai N. et al. Postpartum depression – identifying risks and access to intervention. Curr Psychiatry Rep. 2022;24(12):889-96. DOI: http://doi.org/10.1007/s11920-022-01392-7
21. Segamarchi PC, Mateus VL, Osório AAC. Mental health of postpartum women during the COVID-19 pandemic in Brazil. Psicol Teor Prát. 2023;25(2):ePTPCP14807. https://doi.org/10.5935/1980-6906/ ePTPCP14807.en
22. Çankaya S, Simsek B. Effects of antenatal education on fear of birth, depression, anxiety, childbirth self-efficacy, and mode of delivery in primiparous pregnant women: a prospective randomized controlled study. Clin. Nurs. Res. 2020;30(6):818-29. DOI: http://doi.org/10.1177/1054773820916984
23. Mateus V, Cruz S, Costa R, et al. Rates of depressive and anxiety symptoms in the perinatal period during the COVID-19 pandemic: comparisons between countries and with pre-pandemic data. J. Affect. Disord. 2022;316:245-53. DOI: https://doi.org/10.1016/j.jad.2022.08.017
24. Mesquita A, Costa R, Bina R, Cadarso-Suárez C, et al. A cross-country study on the impact of governmental responses to the COVID-19 pandemic on perinatal mental health. Sci Rep. 2023;13(1):2805. DOI: 10.1038/s41598-023-29300-w
25. Muller EV, Martins CM, Borges PKO. Prevalence of anxiety and depression disorder and associated factors during postpartum in puerperal women. Rev Bras Saude Mater Infant [Internet]. 2021;21(4):995–1004. DOI: https://doi.org/10.1590/1806-93042021000400003
26. Quevedo LA, Scholl CC, Matos MB, et al. Suicide Risk and Mood Disorders in Women in the Postpartum Period: a Longitudinal Study. Psychiatr Q. 2021;92(2):513-22. DOI: https://doi.org/10.1007/s11126-020-09823-5
27. Passos JA, Arrais AR, Firmino VHN. Saúde mental na perinatalidade: perspectivas de usuárias e profissionais da Atenção Primária à Saúde. Com. Ciências Saúde. 2020;31(1):161-178. Available from: https://bvsms.saude.gov.br/bvs/periodicos/ccs_artigos/saude_mental_perinatalidade.pdf
28. Zaldivar AP, Prates LA, Perez RV, Gomes NS, Pilger CH. Couples experiences about the partner’s participation in the puerperium. RSD [Internet]. 2020;9(7):e913974510. DOI: https://doi.org/10.33448/rsd-v9i7.4510
29. Gonçalves FBAC, Almeida MC. A atuação da enfermagem frente à prevenção da depressão pós-parto. Ensaios Ciência [Internet]. 2019;23(2):140-47. DOI: https://doi.org/10.17921/1415-6938.2019v23n2p140-147
30. Santana GW, Maurique LS, Gomes RM, Normando LV, Ferrari IS, Suarez CSM, et al. Prevalência e fatores de risco da depressão pós-parto no Brasil: uma revisão integrativa da literatura. Debates em Psiquiatria [Internet]. 2022;12:1-23. DOI: https://doi.org/10.25118/2763-9037.2022.v12.376
31. Oliveira JE, Ferrari AP, Tonete VLP, et al. Resultados perinatais e do primeiro ano de vida segundo cor da pele materna: estudo de coorte. Rev Esc Enferm USP. 2019;53:e03480. DOI: http://dx.doi.org/10.1590/S1980-220X2018003903480
32. Prandini NR, Souza SRRK, Resende ACAP, Freitas EAM, Serrato JT, Skupien SV. Salud mental de puérperas durante la pandemia de covid-19: revisión integradora. Aquichan [Internet]. 2022;22(2):e2227. DOI: https://doi.org/10.5294/aqui.2022.22.2.7
33. Theme Filha MM, Ayers S, Gama SGN, Lea MC. Factors associated with postpartum depressive symptomatology in Brazil: The Birth in Brazil National Research Study. J Affect Disord. 2016;194:159-67. DOI: https://doi.org/10.1016/j.jad.2016.01.020 PMid:26826865
34. Hamzehgardeshi Z, Omidvar S, Amoli AA, Firouzbakht M. Pregnancy-related anxiety and its associated factors during COVID-19 pandemic in Iranian pregnant women: a web-based cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):208. DOI: https://doi.org/10.1186/s12884-021-03694-9
35. Silva ALM, Oliveira AS, Ruas BJS, Barbosa LPLP, Landim MEPA, Bruno RR, Freitas SSF, Santos TM, Fernandes TP, Roza TCBN. Os impactos no pré-natal e na saúde mental de gestantes durante a pandemia de COVID-19: uma revisão narrativa. REAC [Internet]. 2021;34:e8633. DOI: https://doi.org/10.25248/reac.e8633.2021
36. Marçal AA, Silva CDC, Cortez EM, et al. Assistência do enfermeiro à mulher com depressão pós-parto: uma revisão narrativa da literatura. Res. Soc. Dev. 2023;12(6):e19512642278. DOI: https://doi.org/10.33448/rsd-v12i6.42278
37. Sampaio AKF, Faria RR, Castro SDM de, Lima RN. Assistência de enfermagem na depressão pós-parto. Rease [Internet]. 2023;9(8):135-45. DOI: https://doi.org/10.51891/rease.v9i8.10794
38. Miguel MF, Ramos CO, Siqueira SMC, et al. Assistência do enfermeiro a mulheres com indícios de depressão pós-parto. Rev. Saúde.Com. 2017;13(4):1088-94. DOI: https://doi.org/10.22481/rsc.v14i1.530
Funding and Acknowledgments:
Nothing to declare
Conflict of Interest Statement
Nothing to declare.
Authorship criteria
Kelvin Leandro Marques Monçalves, Cláudia Zamberlan, Keity Laís Siepmann Soccol: 1,2,3
Josiane Lieberknecht Wathier, Andressa da Silveira, Júlia Oliveira Silveira, Josi Barreto Nunes, Larissa Bertoldo Vagner: 2,3
Scientific Editor: Ítalo Arão Pereira Ribeiro. Orcid: https://orcid.org/0000-0003-0778-1447
Rev Enferm Atual In Derme 2026;100(1): e026013